Illiotibial Band (IT Band) Syndrome
By CEO Robert Forster, PT Lateral knee pain is one of the most common complaints from marathon runners as they build up the mileage in training to above 12-15 miles in preparation for marathon. In most cases, the pain is in one knee and not the other, and this begs the question: why would only one knee hurt if both legs ran the same mileage? The answer, as in all asymmetric overuse injuries, is a mechanical deviation in one or more of the joints of the lower extremity or pelvis on one side or the other. Joint mechanics can be corrupted by an old injury such as an ankle sprain or hamstring strain, or by a pelvic mal-alignment causing a leg-length discrepancy. When the pelvis, which is comprised of two independent large bones call the ilium, is out of line, the joints of the “short” or “long” leg will make adjustments to compensate. The most common compensation is that the foot on the long side will over-pronate as a strategy to flatten the arch and functionally shorten that leg, while the foot on the short side will typically supinate in an attempt to hold that arch up and functionally elongate that leg. These subtle but significant compensations alter joint mechanics and cause aberrant forces to bear down on vulnerable tissues including tendons, ligaments, fascia, and bursa. An effective rehabilitation program must not only treat the painful area but also address the cause of injury by exposing and correcting the mechanical imbalance creating the excessive forces to bear down on the inured structure. Anatomy and Function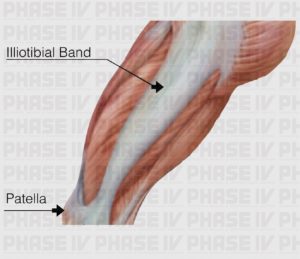 The illiotibial band is a thick band of fascia that extends from the pelvis down along the outside of the thigh to attach below the knee on the outside of the lower leg bone called the tibia. The IT band functions to stabilize the thigh bone and knee during the weight bearing “stance” phase of the running gait, and helps guide the lower leg as it swings forward through the air in the swing phase. Just before foot strike, the illiotibial band slides over a bony prominence on the outside of the knee called the lateral epicondyle. A structure called a bursa (a fluid filled sac much like an internal blister that is suppose to be there) prevents friction between the bony prominence and the illiotibial band.
Pain Presentation
Illiotibial band problems may present at one end or the other of this broad band of fascia running along the outside of the thigh: either at the top, where it originates on the lateral aspect of the pelvis, or much more commonly at the lower end at the site of the bursa on the outside of the knee. This lower IT band pain tends to appear suddenly on a run, and it often becomes so severe that you have to limp or stop the workout and walk home. While it does not represent a high degree of damage to the bursa, or to the IT band, it can be one of the most painful conditions runners suffer and it will stop you in your tracks. If you ignore the pain and continue to run, the pain will progress to daily activities including stairs, squatting, and pivoting.
At the top of the IT band where it attaches to the outside of the ilium and the surrounding muscles, the pain can come on more gradually and is typically much less intense, but can be equally as persistent. Pain in either the top or the bottom should never be ignored because these injuries can be very stubborn and difficult to resolve if you run through the pain for weeks or months.
Differential Diagnosis
Pain at the lateral aspect of the knee can also represent a tendonitis of the popliteus muscle, which often accompanies IT band syndrome or can exist in isolation. Lateral knee pain can also represent a torn lateral meniscus, the cartilage disc between the thigh bone (femur) and the shin bone (tibia).
To determine if your lateral knee pain involves the popliteus muscle-tendon complex, consider if the pain is worse with downhill running specifically. This is the tell-tail sign of popliteus tendonitis. Also, if you feel pain and tightness at the top of the calf on the outside edge, it may implicate this muscle as the painful structure. Symptoms of a torn lateral meniscus on the other hand include clicking, locking, and buckling of the knee. If you have received treatment for what was presumed to be an IT band pain located outside the knee, or have received an injection for the IT band and it did not reduce the pain even temporarily, then consider these other possible diagnoses and seek treatment from an experienced physical therapist. Rehab for a torn meniscus or popliteus muscle-tendon condition is beyond the scope of a self-help injury guide like this.
However, if your pain is at the top end of the IT band along the outside edge of the pelvis, which usually begins more gradually as a subtle ache that becomes worse at the end of the run and after longer runs, it may resolve with the treatment techniques outlined in the Rehabilitation Grid. This can become more severe and begin to hurt during daily activities and when laying on that side in bed.
The Mechanism of Injury
The most common cause of IT band syndrome is a leg-length discrepancy and the compensatory over-pronation of the long-side foot. With over-pronation, the arch on that foot will collapse, essentially shortening the leg to lower that side of the pelvis and even up the leg length inequality to keep the spine straight and the head level. When the foot over-pronates, it causes the lower leg bone to excessively internally rotate late in the stance phase and irritates the bursa as the angle of IT band is altered.
If the lateral knee pain is symmetrical, i.e. occurs bilaterally at the outside of both knees, it may be because you are somewhat bowlegged. This places more stress on the IT band as it slides past the bony prominence on the outside of the knee. Likewise, if the IT bands are tight the bursa can easily become inflamed.
Over time, the bursa becomes inflamed and swollen and causes even more impingement between the IT band and the lateral epicindyle outside the knee. The pain typically limits running rather quickly before it can cause significant damage to the bursa or the illiotibial pain. However, if pain causes you to alter your gait in an effort to limit the pain, you are likely to cause excessive stress on other structures and cause additional, potentially more damaging injuries.
Rehabilitation
The primary approach to all IT band syndromes is to address the inflammation and pain at the injury site while simultaneously working to limit the amount of pronation in the foot when you run. Ultimately this involves correcting leg length inequality with stretching and strengthening exercises. This takes some time, but improving running gait mechanics can immediately start to reduce the pain. To limit over-pronation in your gait, simply increase your cadence or stride frequency – in short, take more steps per minute. Shorter, faster steps not only result in your leg landing more efficiently under your center of gravity, but shorter faster steps also translate to each foot spending less time on the ground during each step. This reduces the time your foot has to pronate and limits the degree of pronation in each step.
In addition to performing stretching and strengthening exercises to address the pelvic misalignment and other mechanical deviations in the lower extremity, the foam roller will speed up your recovery by breaking up muscular adhesions and mobilizing scar tissue in the muscles and the IT band to help correct the dysfunctional mechanics.
If an increased cadence and attempts to achieve a leg length correction do not alleviate the pain, then a more stable shoe with motion control and/or orthotic devices in your shoes may be necessary.
The illiotibial band is a thick band of fascia that extends from the pelvis down along the outside of the thigh to attach below the knee on the outside of the lower leg bone called the tibia. The IT band functions to stabilize the thigh bone and knee during the weight bearing “stance” phase of the running gait, and helps guide the lower leg as it swings forward through the air in the swing phase. Just before foot strike, the illiotibial band slides over a bony prominence on the outside of the knee called the lateral epicondyle. A structure called a bursa (a fluid filled sac much like an internal blister that is suppose to be there) prevents friction between the bony prominence and the illiotibial band.
Pain Presentation
Illiotibial band problems may present at one end or the other of this broad band of fascia running along the outside of the thigh: either at the top, where it originates on the lateral aspect of the pelvis, or much more commonly at the lower end at the site of the bursa on the outside of the knee. This lower IT band pain tends to appear suddenly on a run, and it often becomes so severe that you have to limp or stop the workout and walk home. While it does not represent a high degree of damage to the bursa, or to the IT band, it can be one of the most painful conditions runners suffer and it will stop you in your tracks. If you ignore the pain and continue to run, the pain will progress to daily activities including stairs, squatting, and pivoting.
At the top of the IT band where it attaches to the outside of the ilium and the surrounding muscles, the pain can come on more gradually and is typically much less intense, but can be equally as persistent. Pain in either the top or the bottom should never be ignored because these injuries can be very stubborn and difficult to resolve if you run through the pain for weeks or months.
Differential Diagnosis
Pain at the lateral aspect of the knee can also represent a tendonitis of the popliteus muscle, which often accompanies IT band syndrome or can exist in isolation. Lateral knee pain can also represent a torn lateral meniscus, the cartilage disc between the thigh bone (femur) and the shin bone (tibia).
To determine if your lateral knee pain involves the popliteus muscle-tendon complex, consider if the pain is worse with downhill running specifically. This is the tell-tail sign of popliteus tendonitis. Also, if you feel pain and tightness at the top of the calf on the outside edge, it may implicate this muscle as the painful structure. Symptoms of a torn lateral meniscus on the other hand include clicking, locking, and buckling of the knee. If you have received treatment for what was presumed to be an IT band pain located outside the knee, or have received an injection for the IT band and it did not reduce the pain even temporarily, then consider these other possible diagnoses and seek treatment from an experienced physical therapist. Rehab for a torn meniscus or popliteus muscle-tendon condition is beyond the scope of a self-help injury guide like this.
However, if your pain is at the top end of the IT band along the outside edge of the pelvis, which usually begins more gradually as a subtle ache that becomes worse at the end of the run and after longer runs, it may resolve with the treatment techniques outlined in the Rehabilitation Grid. This can become more severe and begin to hurt during daily activities and when laying on that side in bed.
The Mechanism of Injury
The most common cause of IT band syndrome is a leg-length discrepancy and the compensatory over-pronation of the long-side foot. With over-pronation, the arch on that foot will collapse, essentially shortening the leg to lower that side of the pelvis and even up the leg length inequality to keep the spine straight and the head level. When the foot over-pronates, it causes the lower leg bone to excessively internally rotate late in the stance phase and irritates the bursa as the angle of IT band is altered.
If the lateral knee pain is symmetrical, i.e. occurs bilaterally at the outside of both knees, it may be because you are somewhat bowlegged. This places more stress on the IT band as it slides past the bony prominence on the outside of the knee. Likewise, if the IT bands are tight the bursa can easily become inflamed.
Over time, the bursa becomes inflamed and swollen and causes even more impingement between the IT band and the lateral epicindyle outside the knee. The pain typically limits running rather quickly before it can cause significant damage to the bursa or the illiotibial pain. However, if pain causes you to alter your gait in an effort to limit the pain, you are likely to cause excessive stress on other structures and cause additional, potentially more damaging injuries.
Rehabilitation
The primary approach to all IT band syndromes is to address the inflammation and pain at the injury site while simultaneously working to limit the amount of pronation in the foot when you run. Ultimately this involves correcting leg length inequality with stretching and strengthening exercises. This takes some time, but improving running gait mechanics can immediately start to reduce the pain. To limit over-pronation in your gait, simply increase your cadence or stride frequency – in short, take more steps per minute. Shorter, faster steps not only result in your leg landing more efficiently under your center of gravity, but shorter faster steps also translate to each foot spending less time on the ground during each step. This reduces the time your foot has to pronate and limits the degree of pronation in each step.
In addition to performing stretching and strengthening exercises to address the pelvic misalignment and other mechanical deviations in the lower extremity, the foam roller will speed up your recovery by breaking up muscular adhesions and mobilizing scar tissue in the muscles and the IT band to help correct the dysfunctional mechanics.
If an increased cadence and attempts to achieve a leg length correction do not alleviate the pain, then a more stable shoe with motion control and/or orthotic devices in your shoes may be necessary.








