
By Shelby Stoner, PHASE IV Exercise Physiologist
If you’ve ever experienced chronic knee pain, you know how debilitating it can be. You can’t do your regular workouts, wear your favorite shoes or even walk to the grocery store without excruciating pain. It would make sense to think that the pain is coming from your knee, however, you may be overlooking one of the most common sources of knee pain – that’s not from your knee at all.
IT Band Syndrome is one of the most common overuse injuries among runners. It occurs when the IT band, the ligament that runs down the outside of the leg from the hip to below the knee, is tight or inflamed. The IT band has an attachment at the knee to help stabilize and move the joint. However, when the IT band isn’t working properly, movement of the knee (and of course running) can become extremely painful. Because the most notable symptom is typically swelling and pain on the outside of the knee, many runners mistakenly think they have a knee injury. The pain can be severe enough to completely sideline a runner for weeks, or even longer.
You can read more about the anatomy and diagnosis of IT Band Syndrome in the following excerpt from Healthy Running Step by Step by Robert Forster, Physical Therapist to Olympic Champions and Roy M. Wallack, Los Angeles Times Fitness Columnist.
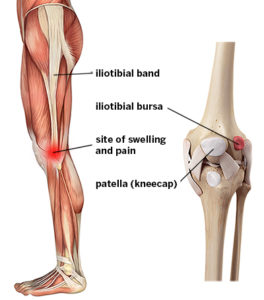
Source: Hospital for Special Surgery
Chapter 9: Rehabbing Running Injuries
Iliotibial (IT) Band Syndrome: Anatomy and Function of the IT Band
An Excerpt from “Healthy Running Step by Step” by Robert Forster, P.T. & Roy M. Wallack
The IT band is a thick band of fascia that extends from the pelvis down along the outside of the thigh to below the knee, attaching on the outside of the lower leg bone (the tibia). The IT band functions to stabilize the thigh bone and knee during the weight-bearing “stance” phase of the running gait and helps guide the lower leg as it swings forward through the air in the “swing” phase. Just before foot strike, the IT band slides over a bony prominence on the outside of the knee called the lateral epicondyle. An internal structure called a bursa (a fluid-filled sac that looks like a blister) prevents friction between the bony prominence and the IT band.
HOW YOU FEEL THE PAIN
Iliotibial band problems can occur at one end or the other: at the top, where it originates on the lateral side of the pelvis, or more commonly at the lower end, at the site of the bursa on the outside of the knee. This lower IT band pain tends to appear suddenly on a run, and it often becomes so severe, you have to limp or stop the workout and walk home. Although it does not represent a high degree of damage to the bursa or the IT band itself, it can be one of the most painful conditions runners suffer. If you ignore the pain and continue to run, the pain will progress to daily activities such as stair climbing, squatting, and pivoting. At the top of the IT band, where it attaches to the outside of the pelvis bone (the ilium) and the surrounding muscles, the pain can come on more gradually. Although less intense up there, it can be equally persistent. Pain in either the top or the bottom of the IT band should not be ignored. The problem can be very stubborn and difficult to resolve if you run through the pain for weeks or months.
DIFFERENTIAL DIAGNOSIS
Lateral knee pain can also represent a tendonitis of the popliteus muscle, which often accompanies IT band syndrome or can exist in isolation. Pain here can also be from a torn lateral meniscus, the cartilage disc between the thigh bone (femur) and the shin bone (tibia).To determine whether your lateral knee pain involves the popliteus muscle-tendon complex, try to determine whether the pain is worse during downhill running, the telltale sign of a popliteus tendonitis. Also, if you feel pain and tightness at the very top of the calf on the outside edge, it may implicate this muscle as the injured structure. Symptoms of a lateral meniscus tear include clicking, locking, and buckling. If you receive an injection for the IT band, and it does not reduce the pain even temporarily, then consider these possible diagnoses and seek treatment from an experienced physical therapist. Rehab for these conditions is beyond the scope of a self-help injury guide like this. However, if your pain is at the top end of the IT band along the outside edge of the pelvis, which usually begins more gradually as a subtle ache that is worse at the end of the run and after longer runs, a do-it-yourself rehab, as outlined in the matrix (see pages 194–195), will most likely work to alleviate the pain.
HOW THE INJURY HAPPENS
If the lateral knee pain is symmetrical (i.e., it occurs bilaterally at the outside of both knees), it may be because you are somewhat bowlegged (technically, genu varum; see alignment evaluation on page 101). Bowleggedness places more stress on the IT bands, which have less clearance to slide past the bony prominence on the outside of a knee called the lateral epicondyle. Likewise, if the IT bands are tight, the bursa can easily become inflamed. The most common cause of IT band syndrome is overpronation of the foot. When the foot overpronates, it causes excessive internal rotation of the lower leg bone late in the stance phase, which alters the angle of pull of the IT band and irritates the bursa. If the IT band pain is unilateral (i.e., only on one side), it might be that one foot is pronating more than the other as an adaptation for a long leg on that side (see page 99 regarding leg-length discrepancies). With overpronation, the arch on that foot will collapse, essentially shortening the leg to lower that side of the pelvis and even up the leg-length inequality, which will keep the spine straight and the head level. Since the lower end of the IT band moves back and forth when the knee bends and straightens with every step, and it hinges from its upper attachment at the pelvis, any deviation in alignment of the pelvis has the potential to change the angle or pull an IT band and create friction at the bursa as well. For instance, if there’s any asymmetry between the two large ilium bones that make up the right and left side of the pelvis, it will alter the angle at which the band glides across the prominence at the outside of the knee and irritate the bursa. Over time, the bursa becomes inflamed and swollen and causes even more impingement between the IT band and the lateral epicondyle. The pain is severe enough that it typically limits running before it can cause significant damage to the bursa or the IT band itself. However, if you respond to the pain by altering your gait in an effort to limit the pain, you are likely to cause excessive stress on other structures and cause additional, potentially more damaging injuries.
REHABILITATION PLAN
The primary approach to all IT band syndromes is to limit the amount of pronation in the foot when you run. And the best way to limit pronation is to increase your cadence or stride frequency—that is, take more steps per minute. Shorter, faster steps not only position your leg to land more efficiently under your center of gravity (see proper running mechanics in chapter 2), but more steps per minute translates to less time your foot spends on the ground each step. This reduces the time your foot has to pronate and limits the degree of pronation. To limit excessive pronation related to a functional leg-length discrepancy, correct the pelvic asymmetry with the stretching and strengthening program in chapters 7 and 8. In the case of a structural leg-length problem (one leg longer than the other), use a shoe lift. In addition to using stretching and strengthening to address long-leg mechanical deviations, use the foam roller to break up muscular adhesions, mobilize scar tissue, and help correct the dysfunctional mechanics. If an increased cadence and leg-length correction do not alleviate the pain, then a more stable shoe with motion control and/or wearing orthotic devices in your shoes may be necessary. Start by using the information in chapter 6 to assess your flexibility and alignment and determine whether you have a leg-length discrepancy. Then follow the rehabilitation strategies outlined in the rehabilitation grid on pages 194–195 to correct deficiencies and resolve the pain.
Read the full book!Healthy Running Step by Step will help runners of all ages and abilities understand the science behind every aspect of running: training program design, running technique, nutrition, recovery, flexibility and strength training and why running injuries occur, how to prevent them, and how to speed up recovery. Injuries plague the majority of runners, wrecking training plans and cutting running careers short by decades, but they are not inevitable. Authors Robert Forster, P.T., and Roy M. Wallack explain that nearly all running injuries can be rehabilitated quicker and even avoided altogether with the right training, strengthening, stretching, running form, and diet strategy. Drawing from Forster’s three decades of training and treating Olympic athletes and more than 10,000 runners at his award-winning Santa Monica, California, physical therapy and high-performance centers, this book emphasizes that better performance is inextricably bound to injury reduction and that a comprehensive, science-based training plan with built-in anti-injury “insurance” must include these crucial elements: Periodization training, Proper technique and footwear, Nutrition, Posture and flexibility, and Strength training. This book also includes detailed, step-by-step rehabilitation matrixes for the five most common running injuries: IT band syndrome, Achilles tendonitis, shin splints, plantar fasciitis, and hamstring injuries. Using these unique matrixes as your guide, you’ll recover from injuries more quickly and understand what you need to do to prevent their reoccurrence.
Pick up your copy of Healthy Running Step by Step today!







